Anatomy and pathophysiology of the intervertebral discs
The intervertebral discs are composed of a pulpous nucleus rich in water and proteoglycans, surrounded by a fibrous ring made up mainly of type I collagen. These structures act as shock absorbers between the vertebrae, keeping the spine flexible. Disc degeneration is a natural process, largely genetically programmed. As a result, the disc gradually loses its water content, reducing its ability to absorb shocks and increasing the risk of cracking of the annulus fibrosus.
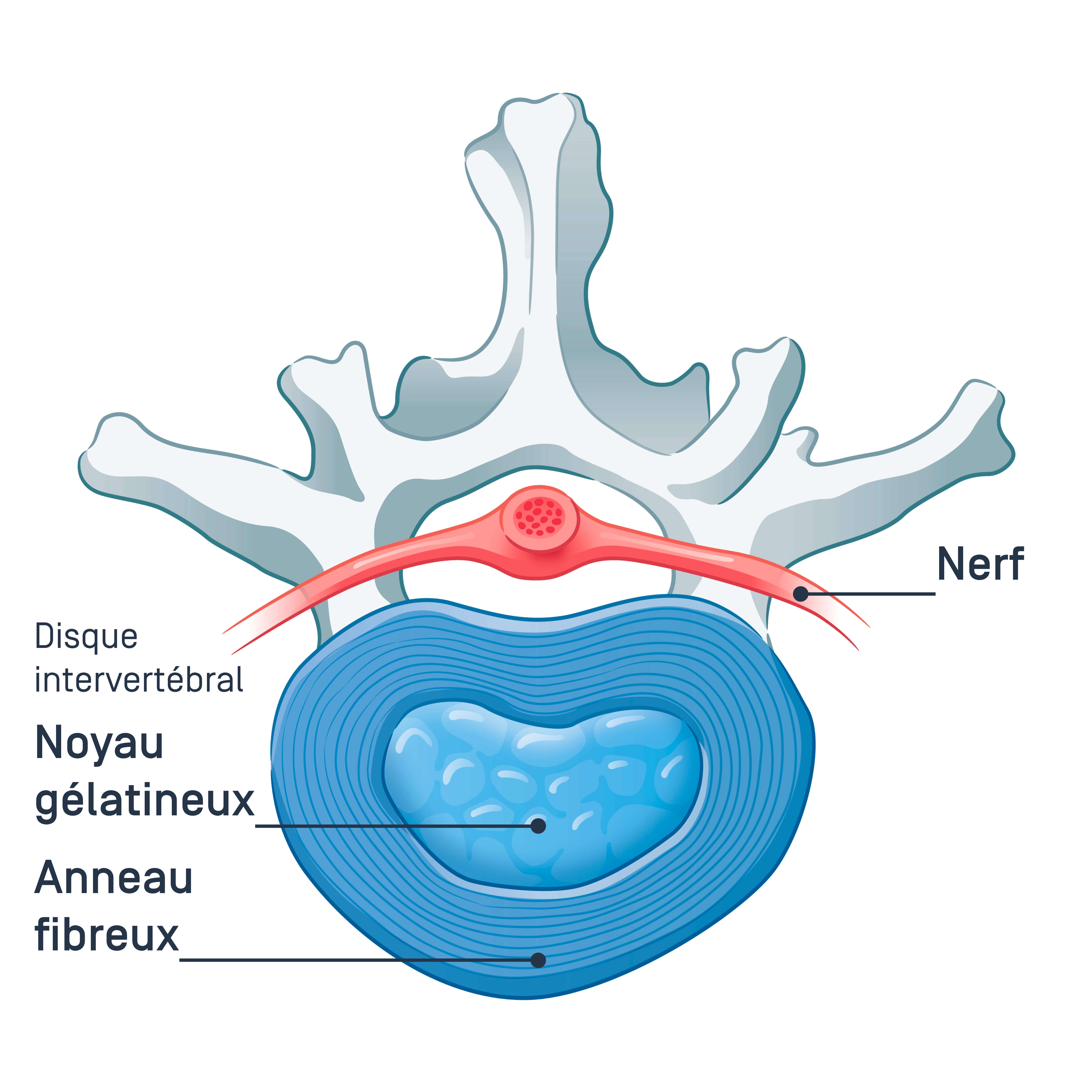
If the annulus cracks, the substance of the nucleus may protrude outside the spinal column (known as a protrusion or protrusion of the nucleus) and may compress a nearby nerve root. This compression causes symptoms that vary depending on the location. The levels most often affected by a herniated disc are L5-S1 and then L4-L5 in terms of frequency, and cause pain along the path of the sciatic nerve, i.e. in the buttock and behind the lower limb, and often as far as the foot. Less frequently, it is the L3-L4 and L2-L3 levels that cause pain in the femoral nerve or cruralgia, i.e. in front of the thigh and often only as far as the knee.
Symptoms of herniated disc
The symptoms of a herniated disc depend on its location and the extent of nerve compression. When a nerve root is affected, radicular pain appears. A herniated lumbar vertebra can cause sciatica, characterised by pain radiating down the back of the leg, or cruralgia, characterised by pain in the front of the thigh. A cervical hernia can cause radiating pain in the arm or shoulder, often associated with tingling and rarely with muscle weakness.
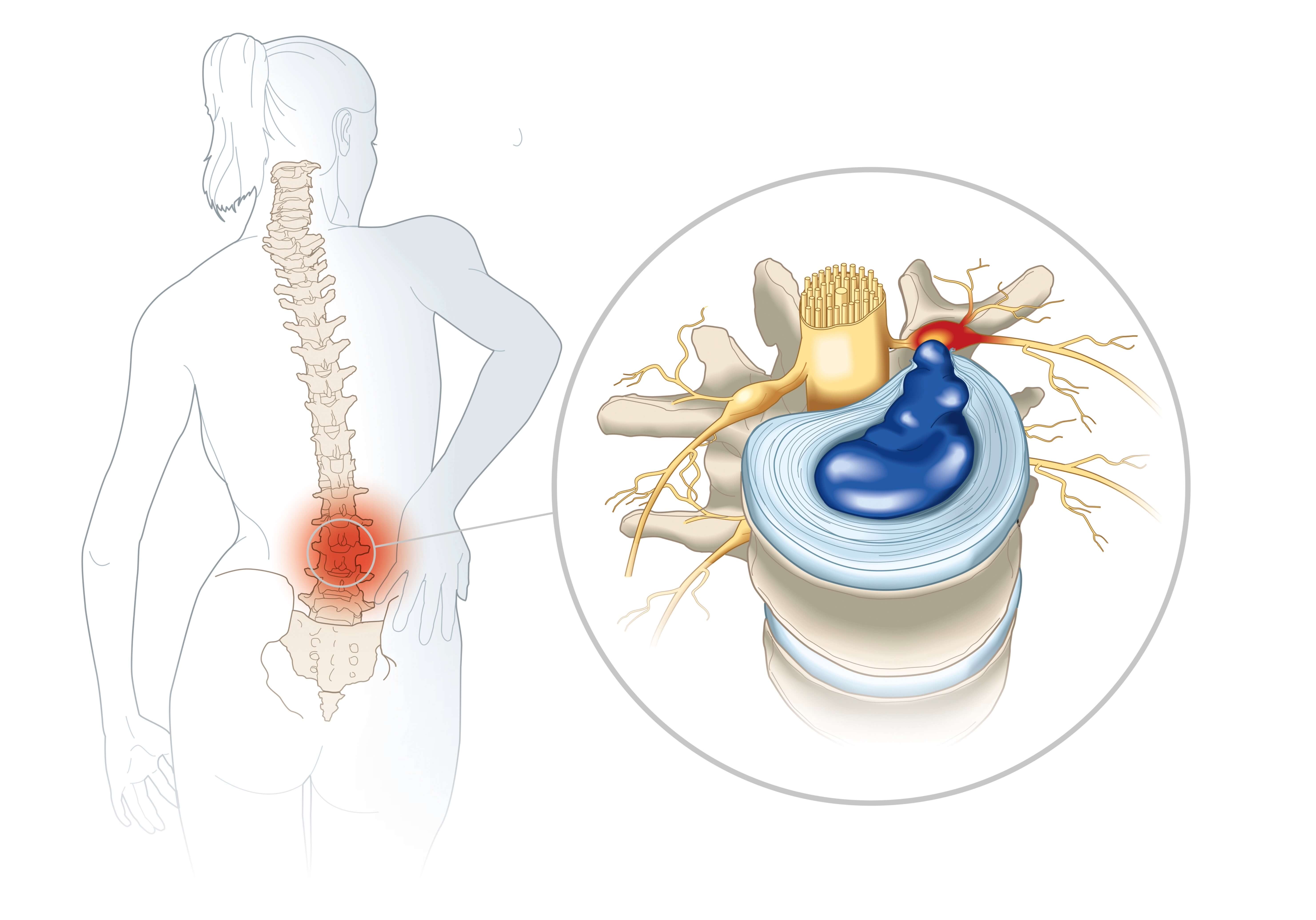
The pain felt follows the path of the compressed nerve. They are sometimes accompanied by tingling and a burning sensation, and may intensify at night, during sleep. If the inflammation associated with the herniated disc takes hold, the pain increases. What's more, as the nerve root is compressed by the protrusion of an intervertebral disc, any movement, coughing or sneezing can awaken or accentuate the pain, as can prolonged sitting. Other possible symptoms are reduced sensitivity in a limb and reduced strength. Serious symptoms are uncommon.
In more than 50% of the normal population, hernias remain asymptomatic and are discovered incidentally during imaging examinations.
Causes and risk factors
Disc herniation is primarily the result of the natural ageing of the intervertebral disc. Genetic factors play a major role in predisposition to disc degeneration. Excessive strain on the back, particularly in certain occupations or strenuous physical activity, may encourage the onset of symptoms, but is not a cause of the ageing of the intervertebral disc
Diagnosing herniated disc
Diagnosis is based primarily on clinical examination. The doctor assesses the osteotendinous reflexes, muscle strength and sensitivity of the affected limbs. Specific tests, such as the Lasègue test for lumbar hernias, can help guide the diagnosis.
Imaging is reserved for persistent cases or cases accompanied by serious neurological signs. MRI is the gold standard for visualising neurological and disc tissues and confirming nerve compression, but it is only indicated in cases of neurological signs or when infiltrations are envisaged. If MRI is contraindicated, a CT scan combined with a myelogram may be performed.
Treating herniated disc
In the majority of cases, a herniated disc can be treated conservatively. This treatment is based mainly on a combination of medication, physiotherapy and adaptation of daily activities. Medication includes painkillers and non-steroidal anti-inflammatory drugs, supplemented in some cases by corticosteroid injections to reduce inflammation. Finally, physiotherapy can also be beneficial, and is prescribed on a long-term basis. Sessions include exercises to strengthen the back and abdominal muscles, as well as muscle relaxation and stretching to improve mobility.
At the same time, it is necessary to avoid aggravating movements while maintaining an appropriate level of activity to prevent muscle stiffness.
Surgery is reserved for serious cases, in particular in the presence of cauda equina syndrome, progressive neurological deficits or persistent disabling pain after a few months (sometimes a few weeks if the pain is unbearable) of conservative treatment. The aim is to remove the herniated fragment in order to decompress the nerve structures. It is estimated that only 5% of hernias require surgery.
Evolution and possible complications
Complications from this condition are rare. However, some can occur, such as loss of muscle strength in a limb, paralysis, sphincter problems (loss of urine or faeces) or significant difficulty walking on tiptoes or heels. These signs of aggravation of the herniated disc may make surgery necessary.
Cauda equina syndrome is a rare complication that constitutes a medical emergency. It is characterised by compression of the nerves at the base of the spine and requires emergency surgery.
Preventing herniated disc
Specific prevention of herniated discs remains limited, as they are essentially linked to genetic factors and age. However, there are a number of practices that can help prevent the symptoms of lower back pain and sciatica and help maintain good back health. It is advisable to maintain a balanced weight in order to reduce the pressure exerted on the intervertebral discs. Adopting ergonomic postures, particularly at work, and regular exercise also help to strengthen the muscles that stabilize the spine.
When should you contact the Doctor?
It is recommended that you seek medical advice as soon as possible in the event of severe pain.
Paralysis, sphincter problems (difficulty controlling urination or bowel movements) or severe muscle weakness are signs of nerve damage. This requires an emergency consultation and, often, surgery.
Care at Hôpital de La Tour
A few years ago, a team at Hôpital de la Tour performed a first in French-speaking Switzerland on a patient suffering from lumbosciatica (acute pain in the lower back and lower limb, along the path of the sciatic nerve) caused by a herniated disc: a lumbar herniectomy using biportal endoscopy. This endoscopic technique, which is less invasive than the conventional technique (herniectomy open to the microscope), makes it possible to remove the hernia while facilitating recovery and reducing the pain following the operation.
A non-surgical approach by the Pain Clinic's analgesia team may also be proposed in certain refractory cases, following clinical assessment by the specialist surgeon.