What is preeclampsia?
Preeclampsia is a condition that occurs during pregnancy and is characterized by poor development or reduced vascularization of the placenta (placental vascular insufficiency). The placenta's blood circulation develops from the very start of pregnancy, and it would be the first stages of its development that would not take place normally. Pre-eclampsia associates arterial hypertension (AHT)*(AHT) (values above 140/90 mmHg for women who have never had hypertension) with a sign of suffering in a maternal organ (kidney, liver, brain, blood elements) or a slowdown in fetal growth. These signs can appear as early as the 20th week of pregnancy. Such early forms are rare, and the majority of preeclampsias occur at the end of pregnancy.
As the baby grows, the placenta's role becomes more important, and if the placenta's blood supply is inadequate, it no longer receives sufficient oxygen and suffers. This, combined with the natural aging of the placenta at the end of pregnancy. As a result, the placenta no longer plays its role properly, and will release a number of signals into the mother's bloodstream, to which the mother's body reacts. Pre-eclampsia can manifest itself in a variety of ways (see symptoms below). When the placenta is no longer able to do its work, it can also affect the baby, whose first sign is slowed growth and a reduction in the quantity of amniotic fluid.
In the unborn baby, pre-eclampsia can lead to delayed growth and prematurity (particularly when delivery is induced). In some cases, also rare nowadays, death in utero can occur. Women who have been medically monitored generally give birth to a healthy baby and recover quickly.
HELLP syndrome
This is a form of preeclampsia that combines liver damage with a reduction in blood elements (platelets and red blood cells). The acronym HELLP stands for Hemolysis, Elevated Liver Enzymes, Low Platelet. Prevention and management are the same as for pre-eclampsia.
Symptoms of preeclampsia
The possible symptoms of preeclampsia include headaches, visual disturbances (blurred vision, spots, flashes), hearing problems (tinnitus), nausea and vomiting, rapid weight gain and edema (water retention in the hands, feet and face). These symptoms can appear and progress rapidly.

Risk factors of preeclampsia
Several factors may be responsible for the onset of pre-eclampsia:
- Chronic hypertension
- Obesity
- Diabetes
- Chronic kidney disease
- Autoimmune disease (lupus or antiphospholipid antibody syndrome, for example)
- Primiparity (first childbirth)
Diagnosis of preeclampsia
Pre-eclampsia is diagnosed by a new onset of high blood pressure during pregnancy or after childbirth. In association with a sign of suffering in a maternal organ, or the appearance of delayed growth of the baby. On the mother's side, this may involve the kidneys, with high levels of protein in the urine (proteinuria), the liver, blood elements (low blood platelets) or signs of neurological disorders such as severe headaches or visual disturbances. Very rarely, convulsions, known as eclampsia, may occur.
Prenatal check-ups can be useful for monitoring any sudden changes in the health of the mother or baby:
- Blood pressure
Blood pressure is measured to ensure that it is not too high. A blood pressure equal to or greater than 140/90 is considered high.
- Test d’urine
This ensures that the kidneys are healthy. A urine sample detects excessive protein loss.
- Tests sanguins
Blood tests may be ordered to obtain a complete blood count and assess levels of creatinine (kidney function) and liver enzymes (liver function). Additional tests may also be prescribed to assess the health of the placenta.
- Weight
Weight gain is considered normal during pregnancy, as long as it remains within the normal range. However, swelling of the face as well as the hands and sudden weight gain can sometimes precede the signs of pre-eclampsia.
Placental biomarkers
Lastly, PLGF (Placental Growth Factor) and sFlt-1 are biomarkers of placental health. They are useful for predicting or diagnosing pathology. Indeed, an unbalanced - and particularly an increased - ratio in the levels of these markers generally indicates a risk of pre-eclampsia a few weeks before the first clinical signs appear.
Treating preeclampsia
The only treatment for preeclampsia is childbirth and delivery of the placenta. To protect both the mother and the baby.
In the rarest cases of preeclampsia occurring before term. Pregnancy can be prolonged, with close monitoring of the well-being of both mother and baby. However, premature birth is the safest option when the placenta, on which the baby depends, is too diseased.
To better control high blood pressure, medication is introduced, but the hypotensive drugs offered have no impact on preeclampsia itself, but do reduce the risk of vascular complications for the mother. The World Health Organization recognizes magnesium sulfate as an effective prevention and treatment for eclampsia. It reduces the risk of eclampsia by over 50% and maternal deaths by 46%. Other drugs, such as corticosteroids, can be administered when pre-eclampsia occurs early, to accelerate the maturation of the baby's lungs.
If symptoms are very severe at an early stage of pregnancy (before the 24th week of amenorrhea), termination of pregnancy may be necessary. After delivery, medical follow-up is necessary. It mainly concerns the monitoring and management of blood pressure. It is also important to ensure that the organs that have suffered damage (kidneys, liver, brain, blood elements) are healing properly.
Evolution and possible complications
After preeclampsia, regular medical follow-up is essential. Indeed, women who have suffered from preeclampsia are at greater risk of developing high blood pressure, heart disease, diabetes or kidney disease. Regular screening and prevention of cardiovascular risk factors is essential. In the event of a subsequent pregnancy, there is a risk of recurrence, depending on the severity and timing of the first episode. Here again, screening and prevention are essential.
1st trimester screening
Pre-eclampsia can be detected early:
To find out more about screening for preeclampsia:
Dépister et prévenir la pré-éclampsie au 1er trimestre de la grossesse
Preventing preeclampsia
Non-medicinal prevention
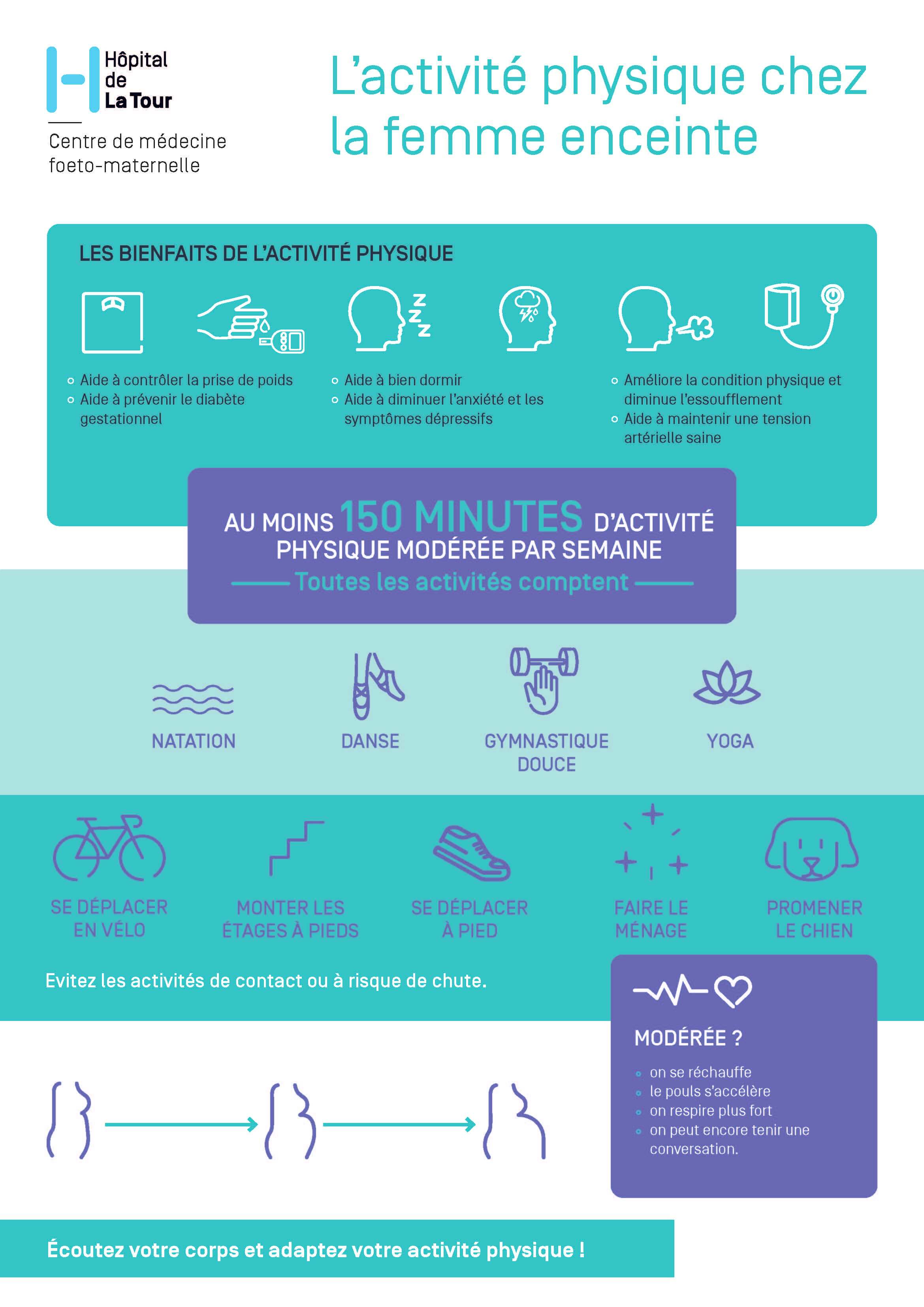
Regular physical activity is safe and significantly reduces the risk of preeclampsia, gestational diabetes, excessive weight gain and pelvic back pain. The benefits of physical exercise during pregnancy are numerous, as it also improves psychological well-being by reducing depressive symptoms and anxiety.
To find out more, discover the sport and pregnancy program.
A Mediterranean-style diet is recommended.
Mental health. Stress, mood disorders and depression require special attention. Psychological well-being contributes not only to personal fulfillment, but also to a better pregnancy and fetal development.
Medication prevention
In certain cases, prevention can be reinforced by prescribing low-dose aspirin for pregnancy as early as the first trimester. However, caution is advised with aspirin, which can only be taken in small doses during pregnancy, on prescription and under medical supervision.
When the diet does not contain sufficient calcium, particularly for high-risk patients, calcium supplements are recommended to prevent preeclampsia.
When should you contact the doctor?
It's important to contact your doctor if you notice any symptoms of preeclampsia.
Care at Hôpital de La Tour
Hôpital de la Tour's maternity unit and maternal-fetal medicine (MFM) center provide effective multidisciplinary, transversal care for high-risk pregnancies. In the event of preeclampsia, the entire medical team is ready to mobilize and take action to care for the mother-to-be and her baby. The Sport and Pregnancy Program, run by the Health and Performance team and physiotherapists at Hôpital de La Tour, offers professional supervision of physical activity during pregnancy.