The ENT are essential structures of the head and neck, often exposed to environmental and behavioural risk factors such as smoking, alcohol or viral infections such as human papillomavirus (HPV). Although these cancers vary in location and manifestation, they share common features in terms of diagnosis, treatment and prevention.
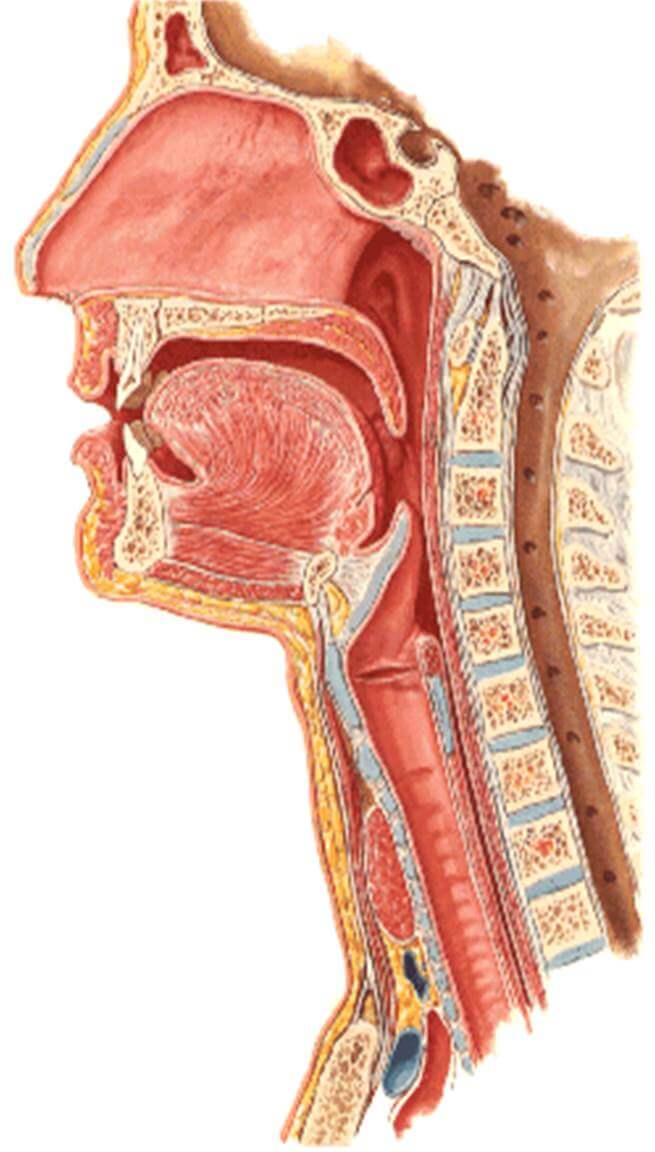
Anatomy of the upper aerodigestive tract
The upper respiratory and digestive tracts (UADT) are the upper part of the respiratory and digestive systems. They ensure the passage of air to the lungs and food to the oesophagus and stomach. They include the nose and sinuses, the oral cavity, the pharynx and the larynx. The salivary glands are functionally associated with the UADT.
Nasal cavities and sinuses
The nasal cavities, connected to the maxillary, frontal, ethmoidal and sphenoidal sinuses, warm and filter the air breathed in, and also play a role in olfaction.
Oral cavity
The oral cavity includes the lips, gums, teeth, tongue, floor of the mouth, cheeks and palate. This region plays a role in mastication, taste and the initiation of digestion.
Pharynx
The pharynx is about 13 cm long and is divided into three parts:
- Nasopharynx: located behind the nasal cavities, it ensures the passage of air.
- Oropharynx: includes the tonsils and the base of the tongue, and is a passageway for air and food.
- Hypopharynx: located behind the larynx, it communicates with the oesophagus.
Larynx
The larynx contains the vocal cords and is essential for breathing, phonation and protecting the respiratory tract against aspiration.
Finally, the main and accessory salivary glands produce saliva, which is necessary for digestion and for moistening the mucous membranes.
Causes of ENT cancers
Cancers of the upper aerodigestive tract (UADT) are influenced by a number of risk factors, often associated. The main identified causes are
Tobacco and alcohol
Tobacco and alcohol are the main causes of cancers of the upper aerodigestive tract. When they are combined, their effect is multiplied by 100, creating a synergistic effect that considerably increases the risk:
Tobacco: over 95% of cases of cancer of the oral cavity, pharynx and larynx are linked to tobacco consumption.
Alcohol: in at least 90% of cases, alcohol consumption is a contributing factor. Alcohol acts as a solvent, facilitating the penetration of the carcinogenic substances contained in tobacco smoke.
Human papillomavirus (HPV)
Certain strains of HPV, notably type 16, are clearly associated with cancers of the oropharynx, including the tonsils and base of the tongue. These cancers often affect younger patients, with a better prognosis than cancers induced by tobacco and alcohol.
Epstein-Barr virus (EBV)
This virus is implicated in undifferentiated carcinomas of the nasopharynx. Although rare in Europe, this tumour is particularly common in South-East Asia and North Africa.
Occupational and environmental factors
Certain occupational environments expose people to carcinogenic substances, such as asbestos, diesel fumes and wood dust. These exposures increase the risk, particularly for nasosinus cancers.
Other factors
- Gastro-oesophageal reflux disease: chronic acid reflux can irritate the mucous membranes and could increase the risk.
- Oral hygiene: poor oral hygiene could also contribute to the development of these cancers.
The different types of ENT cancers
Cancers of the oral cavity often manifest themselves as persistent ulcers or localised pain, and more rarely as bleeding or difficulty chewing. Diagnosis is based on a thorough clinical examination supplemented by a biopsy. Treatment is usually a combination of local surgery and, in some cases, adjuvant radiotherapy.

1. Cancer of the oral cavity
Description and location:
Cancer of the oral cavity includes tumours affecting the lips, tongue, floor of the mouth, cheeks, hard palate and sometimes the gums. These cancers are often linked to chronic irritant factors such as tobacco and alcohol, but can also be influenced by poor oral hygiene.
Specific symptoms:
- Persistent lesions or ulcers in the mouth that do not heal after two weeks.
- Pain when chewing or swallowing.
- Unusual bleeding.
- Persistent bad breath.
- Unexplained tooth mobility or swelling of the cheeks.
Diagnosis:
Clinical examination: Direct observation of lesions with palpation of cervical lymph nodes.
Biopsy: Histological confirmation to confirm the cancer and determine the type of tumour (often squamous cell carcinoma).
Imaging: CT scan or MRI to assess locoregional extension.
Specific treatments:
Surgery: Removal of the lesion with a safety margin.
Radiotherapy: Used as a post-operative adjunct to prevent recurrence, especially in advanced stages.
Chemotherapy: Indicated in combination with radiotherapy in advanced cases.
2. Cancer of the oropharynx
Description and location:
Oropharyngeal cancer affects the soft palate, tonsils, base of the tongue and posterior pharyngeal wall. An increasing proportion of these cancers are linked to infection with the human papillomavirus (HPV), particularly in younger patients.
Specific symptoms:
- Persistent discomfort or pain in the throat.
- Reflex earache (pain radiating to the ear).
- Enlarged cervical lymph nodes.
- Changes in voice
- Dysphagia (difficulty swallowing).
Diagnosis:
Panendoscopy: Investigation of the upper airways with biopsy of suspicious lesions.
MRI: Analysis of locoregional and lymph node extension.
HPV tests: to determine whether the HPV virus is involved in carcinogenesis.
Specific treatments :
Radiotherapy: Often combined with chemotherapy, particularly in the case of HPV-positive tumours.
Endoscopic or robotic surgery: Used for precise exeresis in certain localised cases.
3. Cancer of the hypopharynx
Description and location:
Cancer of the hypopharynx affects the region behind the larynx, including the piriform sinuses and the post-cricoid region. These cancers are often diagnosed late, with a guarded prognosis.
Specific symptoms:
- Progressive dysphagia and pain radiating to the ears.
- Appearance of a cervical mass (metastatic lymph nodes).
- Sensation of a foreign body in the throat.
Diagnosis:
Panendoscopy: Exploration of the upper aerodigestive tract with sampling.
Imaging: CT scan or MRI to assess regional and metastatic involvement.
Specific treatments:
Radical surgery: Often associated with total pharyngolaryngectomy.
Radiotherapy and chemotherapy: Used in combination for inoperable tumours.
4. Cancer of the larynx
Description and location:
Laryngeal cancer includes glottic (vocal cords), supraglottic (above the vocal cords), and subglottic (below the vocal cords) tumours. The main risk factor is smoking.
Specific symptoms:
- Hoarseness or persistent voice changes.
- Dyspnoea (shortness of breath) or breathing difficulties.
- Dysphagia (difficulty swallowing) and neck pain.
Diagnosis:
Laryngoscopy: Allows direct visualisation of lesions.
CT scan or MRI: To assess extension to soft tissue and lymph nodes.
Specific treatments:
Exclusive radiotherapy: For localised glottic tumours.
Total laryngectomy: Indicated in advanced or recurrent cases.
Vocal rehabilitation: Essential after major surgery.
5. Nasopharyngeal cancer
Description and location:
This rare cancer affects the area behind the nasal cavity and is often associated with the Epstein-Barr virus (EBV). It is endemic in parts of Asia and Africa.
Specific symptoms :
- Nasal obstruction, nosebleeds (epistaxis).
- Serous otitis or unilateral hearing loss.
- Cervical swelling due to lymph node metastases.
Diagnosis :
MRI: To assess local extension and metastases.
EBV tests: Serological analysis to confirm involvement of the virus.
Specific treatments :
Conformal radiotherapy: Method of choice for this type of tumour.
Chemotherapy: Added in advanced cases to improve survival rates.
6. Sinus and salivary gland tumours
These rare tumours present with facial pain, nasal obstruction or palpable masses. Diagnosis is made by imaging and cytopsy biopsy. Treatment is essentially based on surgery, sometimes combined with radiotherapy.
Diagnosing ENT cancers
Cancers of the upper aerodigestive tract (UADT) require a precise and structured diagnosis, including a meticulous initial clinical examination followed by in-depth additional investigations. Each stage of the diagnosis is designed to confirm the nature of the tumour, assess its local and regional spread, and guide the choice of treatment.
The initial clinical examination is the first diagnostic step. When a patient presents warning symptoms such as persistent pain in the throat, dysphagia, a change in voice or a cervical mass, the doctor carries out a complete inspection of the ENT sphere. This inspection includes visual observation of the oral and pharyngeal cavities to look for suspicious lesions, combined with palpation of the cervical structures to detect adenopathy.
The clinical examination is often supplemented by indirect laryngoscopy. This examination, performed with a mirror or a nasofibroscope, enables the vocal cords, larynx and neighbouring structures to be examined directly. If a visible or palpable lesion is found at this stage, additional tests are generally carried out to refine the diagnosis.
Complementary examinations, essential for confirming the nature of the tumour and assessing the extent of the disease, mainly include medical imaging and biopsy. A CT scan is often the first-line examination used to map the tumour and assess damage to neighbouring structures. It remains particularly useful for lesions that may affect bone structures. MRI is currently tending to replace CT scanning because of its more precise analysis of soft tissue. In addition, panendoscopy under general anaesthetic is frequently performed. This complete exploration of the aerodigestive tract not only identifies any synchronous tumours, but also allows biopsies to be taken to confirm the histological diagnosis.
Once the diagnosis has been made, the TNM classification is used to stage the disease and guide treatment strategies. This classification is based on three main criteria: the size and local spread of the primary tumour (T), involvement of regional lymph nodes (N) and the possible presence of distant metastases (M). For example, a tumour classified as T1N0M0 is limited and has no lymph node involvement or metastases, whereas an advanced stage such as T4N2M1 indicates an invasive tumour with significant lymph node involvement and distant metastases. This staging is essential for defining the prognosis and adapting treatment options.
Treating ENT cancers
Treatment of ENT cancer is based on a multidisciplinary approach, combining surgery, radiotherapy, chemotherapy and targeted therapies depending on the stage of the disease, the location of the tumour and the patient's general condition.
Surgery
Surgery is the first-line treatment for many ENT cancers. In the case of localised tumours, the main aim of surgery is complete removal of the tumour with sufficient safety margins to minimise the risk of recurrence. For example, for tumours of the oral cavity or oropharynx, partial or total resection of the affected structures may be performed, followed by reconstruction using tissue grafts to restore aesthetic and functional function. In advanced stages, more complex surgery, such as pharyngolaryngectomy, may be required. These operations are often accompanied by cervical lymph node dissection to treat or prevent regional spread.
Radiotherapy
Radiotherapy, often combined or not with surgery, is another mainstay of treatment. It can be used for curative purposes, particularly for early-stage laryngeal cancer, or as a post-operative adjunct to eradicate any residual cells. Modern techniques, such as conformal or intensity modulated radiotherapy (IMRT), enable doses to be concentrated on the tumour while sparing the surrounding healthy tissue. Brachytherapy, a form of internal radiotherapy, is sometimes used for accessible sites such as the tongue or floor of the mouth.
Chemotherapy
Chemotherapy plays a key role in the treatment of advanced or metastatic forms of the disease. It is frequently combined with radiotherapy in concomitant radio-chemotherapy protocols, providing therapeutic synergy. Although these treatments are often effective, they are associated with significant side-effects, requiring management not only during treatment but also in the long term.
Targeted therapies and immunotherapies
Finally, targeted therapies and immunotherapies represent a major advance in the treatment of ENT cancers. Cetuximab, a monoclonal antibody targeting the epidermal growth factor receptor (EGFR), is an option for patients who cannot tolerate conventional chemotherapy. In addition, immune checkpoint inhibitors have shown promising results, particularly for recurrent or metastatic cancers.
These therapeutic strategies, which are often combined, are tailored to the individual patient and discussed at multidisciplinary meetings involving oncologists, surgeons, radiotherapists and other specialists. Personalised care optimises results while minimising long-term sequelae.
When should you contact the Doctor?
In the event of persistent or unexplained symptoms in the head and neck region, it is important to consult a healthcare professional without delay. Patients at risk, such as smokers or regular alcohol consumers, as well as those with a family history of ENT cancers, should be extra vigilant.
Care at Hôpital de La Tour
At Hôpital de La Tour, the treatment of cancers of the upper aerodigestive tract is based on a multidisciplinary approach by a team of specialists with over 30 years' experience in the field. Care is individualised, often with treatments tailored to each patient and his or her cancer. The institution relies on high-performance teams in ablative and reconstructive ENT surgery, including micro-anastomotic flaps. Specialists in radiation oncology use the latest generation of radiotherapy machines to ensure effective treatment while minimising side effects. Oncologists use molecular analyses to propose cutting-edge immunotherapies, personalised for each cancer. Comprehensive monitoring is provided throughout the treatment process, including nutritional and psychological support. Emphasis is placed on patients' quality of life, with post-treatment functional rehabilitation programmes.
Conclusion
Cancers of the upper aerodigestive tract represent a major challenge because of their diversity and their impact on vital functions. Awareness of the symptoms and risk factors, combined with constant advances in treatment, offer better prospects for patients. Today, early management combined with targeted, multidisciplinary treatments can significantly increase the chances of remission, while minimising the functional and cosmetic after-effects.